Copyright © Hans Högman 2021-09-10


Health Care in the Past - Sweden
Childbirth and Midwifery
In the past, all babies were born at home with the
help of a skilled local woman. In Sweden, she was
called a “jordemor” and was the midwife of the
time. A “jordemor” had no formal medical training,
but was an elderly 'wise woman' with experience
and knowledge of childbirth, often passed on from
mother to daughter. The modern term in Sweden
for midwife is “barnmorska”.
Childbirth and childhood illnesses were not without
problems, especially when medical care was not
available. It was not uncommon for pregnant
women to die in childbirth (“död i barnsäng”). One
reason for this was pre-eclampsia (Swe:
havandeskapsförgiftning), which led to high blood
pressure and often a significant amount of protein
in the urine (Swe: äggvita i urinen), which was
serious.
Other complications were cephalopelvic
disproportion, CPD, (Swe: bäckenförträngning) and
exsanguination (Swe: förblödning). After delivery,
infections such as puerperal fever (Swe:
barnsängsfeber) were a problem. In 1750, about 1%
of women delivered died, while in 1850 the figure
was down to 0.5%.
As early as 1708, a form of midwifery training
(barnmorskeutbildning) was started in Stockholm by
the physician Johan von Hoorn, and around 1711 a
midwives' guild was formed. However, before the
opening of the Seraphim Hospital in 1752, a
midwife could only graduate as an apprentice to a
professional colleague. According to the Stockholm
regulations of 1711, the prospective midwife had to
spend at least two years as an apprentice, then
report to a physician and be evaluated by him to
find out whether she was "tenable and capable".
After the apprenticeship, she was graduated from
the Collegium Medicum (A designation for medical
societies with the purpose of supervising the
medical profession).
Towns and cities were urged in 1750 to keep at
least 1 trained midwife. The training was to take
place in Stockholm. However, the licensing
requirement for rural midwives was abolished at
the request of the peasantry just three years later
because the rural parishes did not want to pay for
their midwives to travel to Stockholm.
In Gothenburg and Lund, midwifery training was
introduced at the end of the 18th century. In
Stockholm, the Pro Patria Maternity Hospital
opened in 1774 and the General Maternity Hospital
(Allmänna Barnbördshuset) in 1775, while in
Gothenburg, the Sahlgrenska Hospital opened in
1782 with a maternity ward. The maternity
hospitals (BB) also functioned as training units for
both physicians and midwives.
After childbirth, the mother had to rest and the
Churching of the woman delivered could only take
place until after 6 weeks. Then she was considered
"pure" after childbirth and could be readmitted to
the congregation.
Puerperal fever or childbed fever (barnsängsfeber)
was a bacterial infection that could affect newly
delivered women, usually caused by poor hygiene
during delivery, such as unclean hands and
instruments. The affected woman developed sepsis
(blodförgiftning ) with high fever and rapidly
deteriorating general condition. The mortality rate
was high. When it was realized that higher hygiene
in childbirth was of paramount importance, the risk
of childbed fever decreased significantly. In the
mid-19th century, several discoveries pointed to the
importance of cleanliness in childbirth, for example
in Austria. In Sweden, in 1870, physician Wilhelm
Netzel at the General Maternity Hospital (Allmänna
Barnbördshuset) in Stockholm confirmed that fever
was spread by midwives and doctors carrying
unclean instruments with organic substances. The
hygienic procedures he introduced had a good
effect. In 1879, procedures were tightened and
midwives were required to wash their hands in a
solution of carbolic acid (Phenol) before performing
procedures. For most of the 19th century, science
was aware that bacteria caused many diseases.
Despite this, anti-bacterial treatments were not
available.
In 1867, Englishman Joseph Lister published an
article on antiseptic wound treatment in The
Lancet.
Infant mortality was high. In the mid-17th century,
about one-third of all children died before the age
of 5. By the mid-19th century, however, the figure
was down to a quarter, but that must still be
considered high. An overriding cause was a
nutritional deficiency and poor nutritional status
(often protein deficiency).
In years of famine, this was evident. Pneumonia and
diarrhea diseases were common causes of death.
Diarrhea caused dehydration. Dysentery was a
bacterial intestinal infection that caused severe
bloody diarrhea. Malnutrition combined with
common infections could be devastating for
children. Measles is a viral infection that is normally
not dangerous but which, combined with
malnutrition and poor immunity, could lead to
death. Before antibiotics were available, scarlet
fever could lead to serious and fatal infections.
Physicians
A physician is a person who has graduated from a
university medical school after completing a
professional program. Thereafter, the graduate can
be employed as a doctor. At the beginning of the
19th century, there were about 200 doctors
qualified in Sweden.
In 1800, the population of Sweden was 2,347,303
(Source: SCB).
Physicians existed early in Sweden but they lived in
the cities and were for the rich. Furthermore, their
knowledge was very limited by today’s standard
and no effective medicines such as antibiotics were
available.
Rural areas were largely lacking competent
medical staff. Only in exceptional cases could a
town surgeon or field surgeon be persuaded to
make an arduous and costly journey to see
someone sick in a village.
Instead, peasant society had to rely on old
household remedies that were often mixed with a
large portion of superstition.
It was usually the parish minister or his wife who
had to respond to the sick call, and in the saddle
pocket, the parish minister had suitable medicines
alongside the communion vessels, intended for the
sick person on his deathbed.
The first provincial physicians (provinsialläkare)
began their activities at the end of the 17th century.
In 1774, these activities were nationalized. There
were then 32 provincial physicians, all based in the
towns.
In 1732, when professor Linnaeus made his
Lapland journey, he passed the northernmost
dispensary in the city of Gävle and was the last
provincial physician in the north.
A Provincial physician was a position for medical
officers who acted as district physicians. The title
has been used since the 17th century for
government, especially established medical posts.
An instruction for provincial physicians was issued
in 1744, but the services were only given a fixed
organization by the 1773 Medical Act.
The number of provincial physicians was then 32.
Such services were then (with some exceptions)
available in all the county seats of Sweden. In 1890,
there were 211 provincial physicians and 73 district
physicians (not government physicians) in Sweden.
Provincial physicians thus had a specific station
(place of stationing) and district of service, and their
task was to assist the public with private medical
care. Extra provincial physicians had the same duty
as regular provincial physicians but were paid in full
or in part by municipalities. In each county, there
was also a head provincial physician, paid by the
government, with overall responsibility for the
county's general health care.
In 1973, the term "provincial physician"
(provinsialläkare) was replaced by "district physician"
(distriktsläkare).
Nurses
Nursing education began in 1884 at
Sophiahemmet in Stockholm.
Sophiahemmet opened on 1 October 1889 in
Östermalm, Stockholm. The construction of the
hospital was made possible by a donation from
King Oscar II and his consort Queen Sophia, and
the hospital was named after Queen Sophia.
Sophiahemmet then became Sweden's first private
hospital with a total of 60-70 beds. The hospital
contained housing for 40-50 nurses.
The activities of the Sophiahemmet go back to the
foundation of the "Home for Nurses", which was
inaugurated by Queen Sophia on 1 January 1884.
The aim was to train
nurses.
The image to the right
shows Sophiahemmet
(Sophia Hospital) in
Stockholm in 2006.
Image: Wikipedia.
A nurse trained at Sophiahemmet is called a
"Sophia sister" and they are well known for
maintaining an established uniform, which includes
an apron and cap.
The length of nursing education has historically
varied between one and a half and three years. In
Sweden, professional licensing for
nurses was introduced in 1960, and
the professional title then became
certified nurse (legitimerad
sjuksköterska).
The image to the left shows a so-
called Sophia sister (nurse)
sometime between 1889 and1915.
Image: Wikipedia.
One nurse who has made a great impression in
history is the English woman Florence Nightingale
(1820 - 1910). She is known for her efforts during
the Crimean War (1853 - 1856) where she worked at
a cottage hospital. She succeeded in reducing the
mortality rate in military hospitals in Crimea from
around 42% to 2% by improving the unhygienic
conditions in the hospitals. In 1860 she founded the
Nightingale School of Nursing for nurses in London.
Her work was to influence the work of nurses
around the world.
Hospitals
A hospital (Swe: sjukhus) is an establishment for
primarily inpatient care. An older Swedish term is
“lasarett” (General hospital). Sweden's earliest
monastic hospitals were called “helgeandshus” or
“hospital” and were usually a common gathering
place for the poor and crippled as well as the
mentally and somatically ill of all kinds. Royal
decrees in 1765 and 1776 ordained that county
hospitals (länslasarett) should be established
throughout the realm in combination with special
“kurhus” wards (treatment of venereal diseases).
The image to the right shows
a hospital ward in the past.
Photo Hans Högman, 1998.
Medicinhistoriska museet,
Stockholm (Medical History
Museum).
The first hospital in
Scandinavia, the Akademiska sjukhuset (the
Uppsala University Hospital), was opened in
Uppsala in 1708. In the 1750s there were 6 beds,
and by the turn of the 1800s, the hospital was able
to take 10 patients for clinical care.
In 1752, the Serafimerlasarettet (the Seraphim
Hospital) was inaugurated on Kungsholmen in
Stockholm. The hospital was the first proper
institution in Sweden, dedicated exclusively to the
cure of diseases. It was also the first teaching
hospital in the country. The hospital initially had
only eight beds, but by 1765 the number of beds
had grown to 44.
In Stockholm, Allmänna Barnbördshuset (the
General Maternity Hospital) opened in 1775. At the
time of its opening, it had 17 beds. The maternity
hospitals (abbreviated BB in Swedish) also served
as training units for both doctors and midwives.
In Gothenburg, the Sahlgrenska Hospital opened
in 1782 (founded in 1772 but only opened in 1782).
In Sweden, county hospitals have been called
"länslasarett", while other health care institutions
were called "sjukhus", such as Sabbatsberg Hospital
in Stockholm, Uppsala University Hospital,
Sahlgrenska Hospital in Gothenburg, and Malmö
General Hospital. The 1808 Army Field Medical
Regulations refer to the army's hospitals as
"sjukhus", not "lasarett".
In 1907, there were 75 hospitals in Sweden with a
total of 8,631 beds. In 1907, 79,372 patients had
been treated at these hospitals. Furthermore, at the
same time, there were 73 smaller hospitals and
infirmaries in towns and in countryside with a total
of 999 beds. In 1907, no county lacked hospitals,
most of them had several. The population of
Sweden in 1900 was 5,136,441.
The image to the left
shows an ongoing
treatment of a patient at
the Seraphim Hospital
(Serafimerlasarettet) in
Stockholm in 1898.
Because effective
treatment was often lacking, diseases that are now
easily treatable could often lead to death. Many
diseases were due to poor hygiene often combined
with large crowds. When soldiers were gathered
into armies, more soldiers usually died from
disease than from battles. This was because it was
not known how diseases were transmitted and in
what environment they thrived.
See also History of the Swedish Hospitals
Pharmacies (Apotek)
King Gustav Vasa (1496 - 1560) made the first
attempt to establish an orderly medical system in
Sweden. He acquired physicians and pharmacists
from abroad. The first pharmacy was licensed in
Stockholm in 1575. In 1675 there were 6
pharmacies in the city. In Swede, names of
pharmacies have traditionally been taken from the
fauna.
The image to the right
shows the interior of a
pharmacy in Linköping
at the beginning of the
1900s. Photo Hans
Högman, 2004.
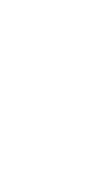
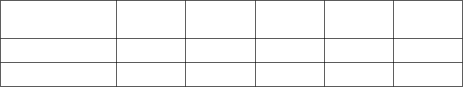
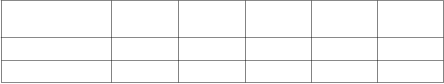
The following chart
shows the growth of pharmacies (Apotek) in
Sweden between 1700 and 1900.





Health Care and Diseases
in the Past (1)
Medical History - Medelpad
Medelpad is a province in central Sweden and its the
major city is Sundsvall.
There was no qualified medical care in Medelpad
before 1726, when Dietrich Theodorus Reineck, a field
surgeon, was employed as city surgeon in Sundsvall.
He was also skilled in the art of midwifery. However,
Reineck left already in 1731, dissatisfied with the
salary.
It was not until 12 years later, in 1743, that
Sundsvall's next city surgeon, Addeus Adde, who was
previously employed as a regimental field surgeon
with the Björneborg Regiment. He held this post until
1766 when his son Fredrik Adde took over as city
surgeon. Fredrik Adde held this post until 1775 when
he was appointed to a similar post in Hudiksvall
town.
In the city of Gävle, there had been a city surgeon
since the end of the 17th century. This post was held
by Carl Pelt between 1709 and 1743.
At this time, Adde and Pelt were the only trained
physicians in the northern half of Sweden, from
Gävle and north and down to Åbo on the Finnish side
of the Baltic Sea. After 1775, when Adde retired,
Gävle was again the nearest town where physicians
were available for the people in Medelpad province.
Carl Pelt settled down after 1743 as a mill owner at
Åvike mill in Medelpad. He had partly inherited the
mill from his father-in-law. He may well be regarded
as the first resident doctor in Medelpad.
Already in the "Medical Order" of 1668, it had been
decided that there should be a provincial physician in
every county of the realm.
The shortage of physicians in Norrland (northern
half of Sweden) had been raised during the
Parliament meeting in 1743 and it was then decided
that the "Senior Master at Härnösand Upper Secondary
School should always be a qualified physician". In 1744
physician Nils Gissler was appointed to this post as
"Provincial-Medicus for the Northern part of
Västernorrland County" which until 1762 included
provinces Gästrikland, Hälsingland, Jämtland,
Härjedalen, Medelpad, and Ångermanland. Gissler
was born in Torp parish in Medelpad.
Gissler organized a corps of assistants by teaching
the parish clerks (Swe: klockare) simple medical care
and bloodletting. It was also common at this time for
priests to have some medical training. Carl Pelt is
said to have been helpful to Gissler in organizing the
medical service in the county.
A few years after Gissler took office, Härnösand got
its first pharmacy. Sundsvall's first pharmacy was
established in 1763. This first pharmacy was called
"Gripen" (The Griffin). A second pharmacy was
opened in 1891 in Sundsvall, "Lejonet" (The Lion).
In 1839, a pharmacy branch was established in
Fränsta to serve the population of western
Medelpad.
When Västernorrland county was divided in 1762,
the county consisted of the provinces Medelpad,
Ångermanland, and Jämtland. Gissler was now
officially authorized as a provincial physician in
Medelpad and Ångermanland.
The city of Sundsvall hired Dr. J Sahlberg as city
physician in 1770, and the following year he was
appointed provincial physician for the whole of
Västernorrland when Gissler died.
Hospitals in Sundsvall
In 1776, during Sahlberg's time, a small hospital
was established in Sundsvall with 2 - 3 beds.
However, the hospital was closed in 1783 when
Sahlberg received Gissler's old lectureship at
Härnösand Upper Secondary School. The movable
assets were moved to Härnösand where a new
hospital was opened in 1788.
During the years of war 1808 - 1809, Sundsvall was
ordered to establish a field hospital. All available
space was used for the hospital. The situation in
Sundsvall was difficult as half the town had burnt
down a few years earlier (1803) and the town was far
from being rebuilt. The field hospital had the most
patients in the autumn of 1809 when over 800
wounded soldiers arrived from Västerbotten County.
Large numbers of soldiers were also stationed in
Sundsvall due to the city's strategic location. Among
these soldiers, field diseases were also rampant.
Some units were reduced by
half.
The image to the right shows
a hospital ward in the past.
Photo Hans Högman, 1998.
Medicinhistoriska museet,
Stockholm (Medical History
Museum).
It was not until 1 January 1844 that a permanent
hospital was opened in Sundsvall. The hospital
was located on Holmgatan and was a two-story
wooden building. The hospital was also an infirmary
for the venereal ill. Between 1861 and 1875, the
number of beds varied between 12 and 28, with a
total of about 80 patients treated per year.
During the 1800s, lumbering expanded considerably.
An exceptionally large amount of people migrated to
Sundsvall to look for jobs with the many lumber
firms in the region; sawmill laborers, loggers, log
drivers, and charcoal makers. The Sundsvall region
became a lumbering Klondike. Sundsvall became the
center of the world’s largest lumber industry district.
The flourishing of the sawmill industry in Sundsvall
during the second half of the 1800s increased the
pressure on the hospital and thus the need for
greater medical resources.
A new hospital was built in Norrmalm district in
Sundsvall in 1875. There was a capacity for 90 beds.
This three-story building was built of timber on a
stone base, contrary to the regulations of the
National Board of Health. The hospital now became
a county hospital.
In the 1880s, there were about 400 patients per year
and one physician. By 1890, the number of patients
had increased to 650 per year and an additional
physician's post was created. The Chief Physician at
this time was Adolf Christierin.
In 1890-1891 extensive improvements and repairs
were made to the hospital. The number of beds was
increased to 120 and electricity was installed in 1902.
In a 1902 inspection by the National Board of Health,
the hospital was described as: "a large wooden
building, poorly sound insulated, inflammable, difficult
to evacuate, and with bedbugs that could not be
eradicated."
In 1905, the construction of a new hospital began. It
was inaugurated on 6 March 1908 and was located
just east of the old operating theatre from the
beginning of the 20th century. The new hospital had
200 beds, 15 of which were for venereal diseases. By
1920 the number of beds had risen to 255. A new
maternity ward with 20 beds was opened in 1927.
In 1956, the number of beds in the hospital reached
714. The hospital remained here until 1975 when a
new hospital was completed in the Bosvedjan district
of Sundsvall.
Sundsvall's municipal administration then moved to
the old hospital buildings.
Since 1853, Sundsvall also had a water spa, located
approximately where the current Badhusparken is.
The town field surgeon's office from 1726 was
withdrawn in 1900 and the last "barber" in Sundsvall
was Bror Ulric Andersson. He is also said to have
been the last in Sweden.
Mental Health Care
In a detached building next to the hospital built in
1875, there was a care institution for the insane.
From the beginning, there were only two beds, in the
1890s six beds, and 1912 eight beds. In 1918, this
building was converted into a maternity ward, and
the mentally ill patients had to be transferred to
other places, including Frösö Mental Hospital.
In a news item in the Sundsvall newspaper, Nya
Samhället in 1910, a consultant from the Swedish
Poor-Law Association tells about a visit to Skön's
poor house. There 11 "fools" were kept, for whom no
more suitable place of residence could be prepared.
Gösta Sundqvist writes in his book "Everything was
not better formerly....." (page 32) "...have seen with my
own eyes these pitiful creatures in their wooden cages
on several occasions ....".
In 1943, the Sidsjön Mental Hospital was opened in
Sundsvall. From 1930, the government had taken
responsibility for the care of the mentally ill. The city
of Sundsvall also ran a municipal mental asylum
from 1916 at Västhagen Hospital. After 1967 it was
transferred to the county council to be used as a
nursing home.
Epidemics in Medelpad
Sundsvall is a seaport town and in maritime towns,
there was in the past always a risk of epidemics
breaking out. In 1812, Sundsvall also obtained the
right of staple towns (the right to trade directly with
foreign countries). This also increased the risk of
epidemics. But it was not only via ships arriving in
Sundsvall that disease could spread but also via the
Norwegian Atlantic coast. In the late 18th century,
peasants from Jämtland province transmitted
venereal diseases from Norwegian seaports.
Jämtland is a Swedish province located west of
Medelpad, by the Norwegian border.
Smallpox arrived in Sweden at the end of the Middle
Ages and an epidemic is known from 1528. Large
outbreaks occurred on and off in Sweden and
throughout Europe during the 18th and 19th
centuries. During an epidemic in 1753, three of Dr.
Gissler's children died. The first smallpox
inoculation in Västernorrland was carried out by Dr.
Gissler in 1761 on 20 children with successful results.
In 1785, a severe epidemic of dysentery ravaged the
whole of Norrland. In 1825, 1833, and 1858,
smallpox epidemics struck Medelpad. Protective
vaccination became compulsory in 1816. It became a
task mainly for parish clerks (klockare) and midwives.
In 1862 Sundsvall was hit by a diphtheria epidemic.
In 1831 a cholera epidemic was feared and a
quarantine master was appointed in Sundsvall. At
the end of the 1830s, a temporary quarantine station
was built on Tjuvholmen, an islet. The epidemic did
not occur in Sundsvall at that time, but in 1850s
cholera came in several rounds. In this epidemic,
about 50 people died.
In 1893, a decree was written that special infirmaries
were to be established in certain parishes as a
precaution against cholera. In Skön parish in
northern Sundsvall, a cholera barrack was set up at
Kabben along the old coastal road. In Granloholm
was Sundsvall's official cholera infirmary.
In the so-called. Petersén's house, west of the small
Büsowska woodland lake, Sundsvall's first epidemic
hospital was established in 1873. This house was
subsequently called the Smallpox House (Kopphuset).
The hospital remained here until 1909 when a new
epidemic hospital was completed on
Ludvigbergsvägen (the Ludvigberg road).
In 1908, when the new hospital was completed, it
was decided that the old hospital would be used by
the Medelpad Tuberculosis Society for the care of
tuberculosis patients. This wooden building was
moved in 1911 to the sanatorium area at Balders
Hage on the North Mountain (Norra Berget). The
building became a school much later. The
tuberculosis hospital had 100 beds. A children's
pavilion was opened in 1931.
According to statistics from the period 1895 - 1900,
various diseases of the respiratory organs were the
most common cause of death in Sundsvall.
In 1918, a severe influenza epidemic spread
throughout the world. It was the Spanish flu (The
Great Influenza epidemic). At the turn of June and July
1918, it arrived in Sweden. In 1919, 200,000 people
fell ill, but the death toll dropped to 9,000.
Sundsvall was also affected and in September 1918 it
reached its peak when 727 cases were reported.
Deaths occurred every day. There was no direct cure.
Food shortages during the Great War, malnutrition
(especially among the urban population), and
consequently low resistance contributed to the rapid
progression of the disease.
Symptoms of the Spanish flu included lower back
pain, high fever, sore throat, severe and rapidly
developing pneumonia, and even heart paralysis.
Many of the epidemics that struck the population
were largely due to poor hygiene and lack of
cleanliness. From 1874 onwards, street sweeping
was organized in Sundsvall. Initially, this task was
carried out by the town bailiff’s office, but from 1881
it was contracted out to a haulage contractor. The
removal of rubbish and latrine from the yards was
arranged so that the hauler was responsible for the
transport at the expense of the property owners. A
water barrel on wheels was also purchased for
watering the streets when the streets were swept.
By 1879, Sundsvall's water and sewage disposal
system had been developed. A few years later, in
1887, the first private water closets came into use.
Related Links
•
Diseases in the past
•
Swedish names of diseases in earlier times
•
History of the Swedish Hospitals
•
Poor Relief in the Past
•
Churching
Source References
•
"Svenska sjukdomsnamn i gångna tider" av
Gunnar Lagerkrantz, tredje upplagan 1988,
utgiven av Sveriges släktforskarförbund.
•
"Vår Svenska Historia" av Alf Åberg, fjärde
upplagan, 1978 (sid 319-321).
•
"Hembygdsforska! steg för steg" av Per
Clemensson och Per Andersson, 1990, (sid 123).
•
"Allt var inte bättre förr .....", Om hälsovård och
sjukvård i Medelpad efter 1700 av Gösta
Sundqvist, 1994
•
Skriften "Sundsvallsbygden" nr 15, årgång 14/97,
artikel "Historiska fakta och berättad
familjehistoria i Sundsvallsområdet" sid 21 av
Barbro Andersson.
•
Skräckens tid, farsoternas historia av Berndt
Tallerud, Prisma 1999.
•
Gamla tiders sjukdomsnamn, Olof Cronberg,
2018.
•
Wikipedia
•
NE, encyclopedia
Top of Page

Until 1970, Swedish pharmacies were run by
individual pharmacists, who had special privileges
from the Crown (so-called apoteksprivilegium), which
were hereditary but used to be transferred by
purchase (privilege trade). In 1970, the entire
pharmacy business was nationalized and
Apoteksbolaget (now Apoteket AB) took over the
business. The pharmacy monopoly ended in autumn
2009, and at the end of January 2010, most of the
pharmacies that were deregulated began to
rebrand.
Medical Treatments
Bloodletting
Bloodletting is an ancient medical treatment. Using a
so-called cup (Swe: “koppa”), blood was drained from
the body which would cause the sickness to come
out through the blood and thus cure the person.
Leeches were also used for bloodletting.
In the 1850s, the use of
bloodletting as a method of
treatment declined sharply.
The image to the right shows an
ongoing bloodletting in Värmland
in 1922. Image: Wikipedia.
Nordiska museet.
The image to the
left shows the
instrument (lancet)
with which one
opened the vein.
According to very ancient theories, the
body contained four fluids; blood,
mucus, yellow bile, and black bile. For good health,
these fluids had to be in balance with each other
and that disease occurred when any of these were
present in too small or large quantities. The theory
was based on the properties of drained blood. The
fluids were thought to reside in various organs of
the body, where they were formed and stored, and
added to the blood.
The yellow bile resided in the liver, the mucus in the
brain, the black bile in the spleen, and the red bile in
the blood. All fluids had to be present in the blood in
the right quantity and strength. It was mainly the
mucus that was thought to cause disease.
Regardless of the cause of a disease, bloodletting
was considered the best way to cure the sick person
by draining the diseased blood with its mucus from
the diseased area of the body.
Before the body's blood circulation was known, it
was thought that blood was locally bound in defined
areas and where blood could become bad from
mucus accumulation. Chills were thought to be a
way for the body to counteract this and that fever
prevented the mucus from congealing and so could
expel it through sweating.
Much superstition has been associated with
bloodletting. In ancient almanacs, there could be
precise instructions as to which part of the body,
ruled by different constellations in the Zodiac, was,
therefore, most appropriate, or inappropriate, to
draw blood from at a particular time for a particular
ailment.
Traits of the signature doctrine also came into play.
For example, bloodletting on young men would
preferably be done when there was a new moon,
while older men would be bloodletting when the
moon was on the wane.
The amount of blood to be drawn was depending on
the patient's age, size, health, and illness. According
to a medieval instruction: From a strong man should
be taken as much blood as a thirsty person can swallow
in one gulp. From a weak person, as much blood as
would fit in an ordinary egg.
It was most common to open veins in the arms.
There were three veins from which blood was
drawn. From the top vein, they would draw blood
partly for prevention and partly to cure headaches.
The middle vein was used to cure heart and lung
diseases. The lower vein was used to treat pain and
diseases of the liver, kidney, and spleen.
The Medical Thermometer
The medical thermometer and fever temperature
curves are aids in medical care. It was not until the
1870s that they came into regular use, mainly
through the German clinician Carl August
Wunderlich (1815 - 1877). By continuously
measuring body temperature, he was able to
establish that temperature curves had a different
appearance depending on the disease. Previously,
the fever had been thought to be a disease in its
own right. Now it was established that fever was
only a symptom, which was a great help in
diagnostics.
The physician Magnus Huss introduced the practice
of regularly measuring the temperatures of the sick
in 1838 at the Seraphim Hospital in Stockholm. It is
not known when medical thermometers began to be
used regularly in Sweden, but eight medical
thermometers were purchased in 1870 at the
Västerås Hospital.
The measurement of body temperature was greatly
simplified with the advent of min/max
thermometers. In Sweden, this happened in the
early 1880s. Swedish production of min/max
medical/clinical thermometers began in 1895.
Stethoscope
A stethoscope is an instrument that propagates
sound from a mouthpiece to the user's ears and can
be used to listen to the heart, lungs, and intestines,
among other things. The first stethoscope was
invented in 1816 by the French physician René
Laënnec and consisted of a
monophonic wooden tube. The first
version of a stethoscope consisted of a
wooden tube about 30 cm long with a
diameter of about 3-5 cm.
The image to the right shows a
wooden stethoscope from the late
19th century. Image: Wikipedia.
Anesthetics
When it comes to anesthetics, there wasn't much
available in the past. Ether was one of the first
anesthetics and began to be used as an inhaled
surgical anesthetic in 1846 in the US, followed the
following year by chloroform.
Ether is a clear, colorless, highly volatile, flammable
liquid with a peculiar aroma and burning taste.
Chloroform is one of the oldest anesthetics used in
surgery. It was considered to have several
advantages over the ether. It was not flammable like
ether and also has a more pleasant smell. However,
towards the end of the 19th century, it was realized
that chloroform tended to cause liver damage, as
well as cardiac arrhythmias and ether, became the
dominant anesthetic. The effect of chloroform is not
immediate; it takes at least five minutes for the
person to lose consciousness.
Anesthesiology is the study of anesthesia and
administering anesthetics. The word anesthesia is
not used very often in everyday Swedish, much
more common is the word narcosis (Swe: narkos)
and an anesthesiologist is usually referred to as a
“nakosläkare”. Anesthesia/narcosis means controlled
sedation together with painkillers.
Antisepsis
In the 1860s, antiseptics, i.e. cleanliness,
sterilization of surgical tools, etc., began to be used
in health care. An antiseptic is a germicide used on a
body surface to kill or inhibit the growth of
microorganisms such as bacteria, fungi, parasites,
and viruses.
Phenol (carbolic acid) was used medically in the past
as a disinfectant in dilute solution, carbolic acid
solution, or carbolic water. When it was realized that
higher hygiene in childbirth was of paramount
importance, the risk of childbed fever decreased
significantly. In 1870, doctor Wilhelm Netzel at the
General Maternity Hospital (Allmänna
Barnbördshuset) in Stockholm was able to establish
that fever was spread by midwives and doctors
carrying organic substances on unclean instruments.
The hygienic procedures he introduced had a good
effect. In 1879, procedures were tightened and
midwives were required to wash their hands in a
solution of carbolic acid before performing
procedures.
In everyday language, antiseptics and disinfectants
are often used interchangeably. However,
disinfectants also include agents used to kill
microorganisms on objects such as tables, floors,
buildings, etc.
Antisepsis aims to combat pre-existing
microorganisms, as opposed to aseptic, which aims
to prevent the emergence of microorganisms, for
example through cleaning and sterilization.
X-Ray Examinations
An X-ray examination is an examination of the
body's bones or internal organs using X-rays. After
developing, any lesions or changes appear on the X-
ray photograph. In the past, the X-ray was also called
radiography and the plates radiogram. Wilhelm
Conrad Röntgen (1845 - 1923) was a German
physicist and the discoverer of X-rays.
X-rays began to be used after 1895.
History of the Penicillin
The Egyptians used mold from bread or porridge as
an antibiotic thousand years ago. In the Swedish
peasant's practice, poultice (Swe: grötomslag) are
listed and if one was left on for a long time, it began
to mold.
A poultice, also called a cataplasm, is a soft moist
mass, often heated and medicated, that is spread on
a cloth and placed over the skin to treat an aching,
inflamed or painful part of the body. It can be used
on wounds such as cuts. The Swedish word
“grötomslag” literally means “porridge wrapping”.
What the porridge is made of is of no great
importance, it can be prepared from ordinary flour,
oatmeal, linseed, or something similar, the
important thing is that it maintains a suitable
temperature to heat without burning or causing any
other discomfort. When the porridge is ready, it is
placed in a cloth folded into a package so that it
does not stick, then the package is placed on the
area in question.
In 1928, Alexander Fleming (1881-1955) discovered
that the mold fungus Penicillium notatum produced a
bactericidal substance. He called it penicillin. In
1939, Ernst Boris Chain and Howard Walter Florey
began experiments to produce large quantities of
penicillin from broth cultures. Its bactericidal effect
was confirmed in large clinical tests in 1942. Mass
production soon began in the US and saved the lives
of tens of thousands of Allied soldiers during World
War II.
The first treatment with penicillin in Sweden took
place at Sabbatsberg Hospital in 1944.
Antibiotics:
Antibiotic means to biologists substances produced
by living organisms for the purpose of keeping other
organisms away. For example, both bacteria and
fungi live either as parasites or by breaking down
dead material. Since both have the same food
source, they try to poison each other by secreting
substances that the other cannot tolerate. For
example, ascomycetous fungi produce penicillin to
keep bacteria at bay, while actinobacteria produce
amphotericin to keep fungi at bay.
The antibiotics that have become known are those
that can be used as medicines. When we talk about
antibiotics in everyday language, we are referring to
drugs against bacteria in general. The drugs can be
either bactericidal (killing) or bacteriostatic
(inhibiting growth).
The first antibacterial drug was mercury, used
against syphilis as early as the 16th century.
However, this was very dangerous for the patient.
In folk medicine, mold has been used since ancient
times as a remedy for various diseases. The first
scientific observation of antagonism between
different microorganisms was made by Louis
Pasteur (1822-1895) and Joubert, who already in
1877 observed that certain aerobic bacteria
inhibited the growth of anthrax bacteria.
Dental Care
Since 1797, a degree has been a requirement for
practicing dentistry in Sweden. Organized dentistry
also began to appear in the 19th century.
Dental care has been available for a long time
through barbers. But now came trained dentists.
However, it was expensive to go to the dentist and it
was a "pleasure" for the wealthy. The anesthetic used
was alcohol. The dental drills used in the late 19th
century were treadle-driven. Only after the turn of
the century did the first electrically powered drills
appear. There were also traveling dentists around
the turn of the century. The first Swedish school
dental clinic was established in Stockholm in 1907.
Folktandvården (Public dental care) is the name
given to the public dental care in Sweden that has
been run by the county councils (Landsting) since
1938. Initially, Folktandvården only provided dental
care for children, but over the years it has expanded
to include both adult and specialist dental care.



Number of Swedish Pharmacies 1700 - 1900

Pharmacies
1700
1750
1800
1850
1900
Stockholm
9
9
12
14
20
Entire country
27
45
95
137
322